Mother’s Day coincides with another special day – the beginning of Food Allergy Awareness Week. May is Allergy Awareness Month, and each year one week is dedicated to food allergy awareness. For 2022, it runs from May 8th to May 14th. Though it hasn’t received as much fanfare these past two years, the Empire State Building is continuing their Food Allergy Awareness tradition. On May 10th, they will glow teal once again. And we’ve forged ahead with an update of our food allergy awareness information and top allergen-free recipes. But remember, awareness shouldn’t be limited to just one week. We encourage you to use and share and use this information any time of the year!
Food Allergy Awareness Week: Over 120 Recipes and Resources
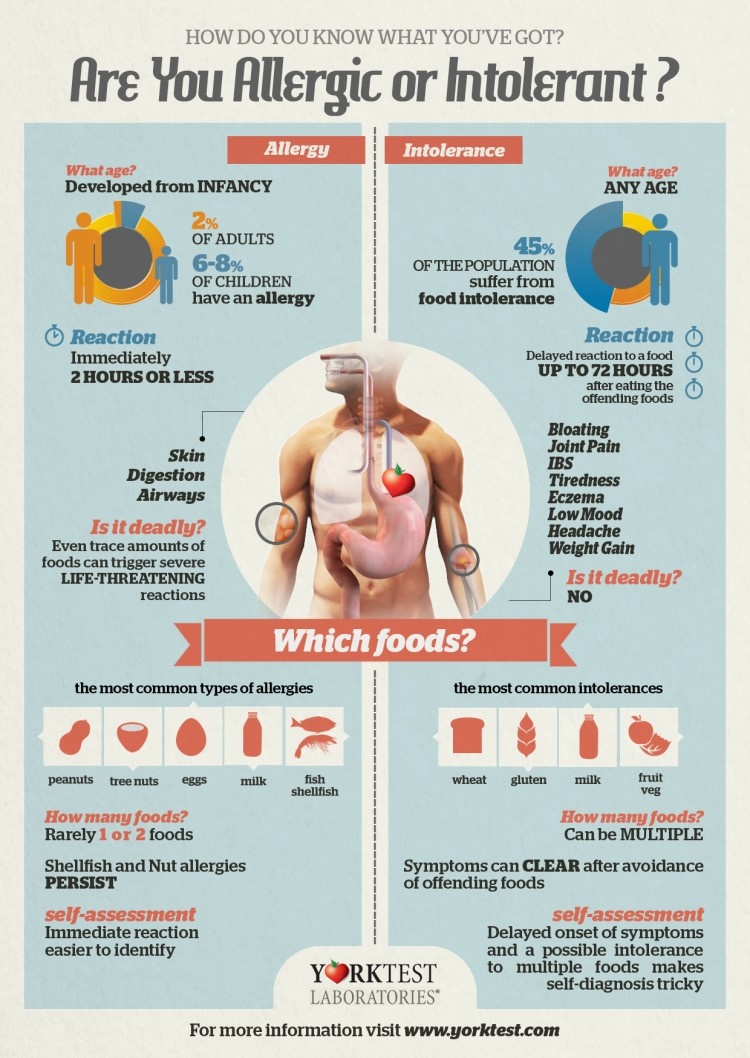
This post includes information to help increase awareness and accommodation of food allergies. It covers the topic of allergies vs intolerances, has dozens of top 8-free recipes, and includes community resources, like awareness printables. This post is for informational purposes only and is not intended to diagnose, treat, or sway you toward any type of diet. If you believe you have any type of food reaction, consult your physician.
Food Allergy, Intolerance, …
Below is a cool diagram that outlines at a glance the differences between what we think of as a classic food allergy and food intolerance.
…or an Allergy that Behaves Like an Intolerance?
But this simple assessment is not the end all be all of possible food reaction issues. Lying somewhere in the middle ground is Eosinophilic Esophagitis (EoE) – a condition that hits home for my family – and Food Protein-Induced Enterocolitis Syndrome (FPIES). Both are immune system reactions to food (like classic food allergies addressed above) but occur specifically in the gastrointestinal tract (like food intolerance). Both EoE and FPIES are typically classified by the medical community as food allergies, but the reaction times may be more delayed and they can onset later in life.
As you may have guessed, milk is a top trigger in all four of the aforementioned food reaction types. For those without an IgE-mediated food allergy reaction (a.k.a. that classic food allergy diagnosis), but who are certain they are reacting to the protein in dairy, not the lactose, EoE and FPIES might be worth looking into. They are both cell-mediated reactions, so traditional IgE testing may not be enough to uncover the issue.
Alisa’s Top 8-Free Recipes
What would Food Allergy Awareness Week be without amazing food? Following are some allergy-friendly and gluten-free recipes that we have enjoyed in my home. All are free of the Top 8 Food Allergens (dairy, egg, wheat / gluten, soy, peanut, tree nut, fish, and shellfish) and for the most are free of the Canadian Top 11 Food Allergens, too!
Top 8-Free Smoothies and Bevies
- Breakfast Blueberry Smoothie
- Mighty Molasses Milk
- Sunbutter & Jelly Smoothie (adapted)
- Light Coconut Milk Creamer
- Tropical Spring Smoothie
- Banana Split Shake
- Homemade Maple Hemp Milk
- Super Pumpkin Spice Protein Shake
- Cherry Chocolate Chip Shake
- Black and Blue Smoothie
- Hot Cocoa made with Water
- Peachy Power Smoothie
- Papaya Mango Shake with Fresh Raspberry Puree
- Sweet Potato Pie Smoothie
- Summer Sunrise Smoothie
- Pomegranate Smoothie
- Cosmic Coconut, Cranberry and Cherry Smoothies
- Chocolate Spice Smoothie
Top 8-Free Breakfasts
- Cream Biscuits and Gravy
- Strawberry Shortcake Waffles (pictured above)
- Jumbo Triple Chocolate Mug Muffins
- Maple & Brown Sugar Steel Cut Oatmeal + Griddle Cakes
- Chocolate Chip Muffin Tops
- The Best Gluten-Free Vegan Pancakes
- Pumpkin Pie Oatmeal
- Mini Maple French Toast Casseroles
- Banana Oat Trail Mix Muffins
- Vanilla Chia Pudding Parfaits (pictured above)
- Cinnamon Roll Pancakes
- Cinnamon Buckwheat French Toast
- Healthy Power Muffins
- Overnight Buckwheat Pancakes
Top 8-Free Meals and Meal-Makers
- Condensed Cream of Mushroom Soup
- Condensed Cream of Celery Soup
- Allergy-Friendly Chicken Nuggets
- Roasted Carrot Bisque
- Cheesy Broccoli “Nachos”
- Creamy Italian-Style Baked Risotto
- Moroccan Roasted Veggie Power Bowls
- Bacon Roasted Brussels Sprouts
- The Best Cheese-less Scalloped Potatoes
- Sticky Coconut Chicken
- Cran-Apple Crunch Chicken Salad w/ Creamy Maple Dressing
- Bechamel / White Sauce
- Apple Cider Vinaigrette Coleslaw
- Honey Mustard Chicken
- Sweet & Sour Roasted Vegetables
- Butternut Pasta with Sage Cream Sauce
- Salt ‘n Pepper Sweet Potato Fries (pictured above)
- Tuna Noodle Un-Casserole
- 7-Layer Salad with Creamy Chipotle Dressing
- Maple-Glazed Kabocha Squash
- Southwestern Stovetop Mac and Cheese
- Cheesy Pepperoni Pizza with Roasted Tomato Sauce (pictured above)
- Homemade Taco Seasoning
- Green Bean Casserole
- Sun-Dried Tomato Pasta with Chicken and Basil
- Creamy Green Garlic Soup
- Vietnamese-Style Lemongrass Chicken Noodle Soup
- Spring Rolls with Spicy Apricot-Ginger Sauce
- Tex-Mex Dinner Night
- Baked Curry Risotto
- Rustic Roasted Eggplant Puttanesca
- Massaged Kale Salad with Pomegranate and Citrus
- 5-Spice Glazed Kabocha Squash
- Buttery Scalloped Potato Stacks
- Easy Cheesy Sauce
- Cream of Celery Root Soup
- Quick Sun-Dried Tomato and Broccoli Penne
Top 8-Free Snacks
- Cheesy Quinoa Bites
- Chewy No Bake Granola Bars
- Caramel Apple Oat Bars (pictured above)
- Mexican 7-Layer Dip
- No Bake Iced Lemon Cookie Granola Bars
- Healthy Caramel Apple Nachos
- Frozen Fruit Pops
- Healthy Vegan Queso Dip
- Maple Spiced Pumpkin Seeds
- Rustic Cinnamon Apple Saute
- Super-Friendly Trail Mix Cereal Bars
- Wholesome Chocolate Chip Cookie Bars
- Triple Chocolate Granola
- Wholesome Chocolate Chip Oatmeal Cookie Dough Balls
Top 8-Free Desserts
- Chocolate Chip Ice Cream
- Every Monster Edible Cookie Dough
- Strawberry Fool Dessert
- Classic Vanilla Coconut Ice Cream
- Mixed Fruit Crisp
- No Bake Power Cookies
- S’mores Ice Cream Sandwiches with Homemade Marshmallow Ice Cream
- Homemade Chocolate Kisses
- Deconstructed Banana Cream Pie Parfaits
- Pumpkin Apple Pie Cake
- Chocolate Truffles
- Mint Chocolate Chip Brownie Pizza
- Whipped Coconut Cream
- Banana Cream Pie 4 All
- Dairy-Free Fantasy Fudge
- Peach Crisp Ice Cream
- Blackberry Lime Yogurt Pops
- Sandwich Cookies with Homemade Icings
- Fudge Bites
- Chocolate Pudding Ice Cream
- Cranberry Pumpkin Bread
- Fudgy No Bake Oat Cookies
- Fresh Strawberry Ice Cream
- Double Chocolate Orange Cookies
- Buttercream Frosting
- Sunbutter and Jelly Ice Cream Sandwiches (adapted)
- Chocolate Pudding with Raspberry Infusion
- Instant Sweetened Condensed Mylk
- Perfect Pumpkin Bread
- Mini Salted Caramel Cupcakes
- Oatmeal Cookie Ice Cream Sandwiches
- Fruit ‘n Crème Ice Pops
- Chocolate-Dipped Strawberries
- Ice Cream Sandwich Cake with Vanilla Whip and Chocolate Cream Filling
- Maple Cream Fudge
- Carrot Cupcakes with Cream Cheesy Frosting
- Strawberries ‘n Cream Chocolate Cups
- Homemade Peppermint Patties
- Multi-Grain Chocolate Chip Cookies
- Chunky Maple Blueberry Sauce
- Hot Chocolate Cookies (pictured above)
- Easy Ice Cream Graham-wiches
Want more? See all 1200+ Top-8 Free Recipes and Reviews!
Visual Guides for Food Allergy Awareness Week
Enjoy and share the infographics, printable posters, bookmarks, and videos below for visual awareness!

- 18 Things To Know About Food Allergy Reactions – A helpful ebook guide from top allergy experts.
- Talking Food Allergies – Snappy Comebacks – This quippy printable offers conversation starters and fast responses to the inevitable food allergy doubters.
- Six that Save Lives – An infographic / poster with the critical and life-saving steps to take during a food allergy emergency.
- Be a PAL Posters and Shareables – The Be a PAL: Protect A Life From Food Allergies education program can help children learn how to be a good friend to kids with food allergies.
- I am a Child with Food Allergies – Cute printable posters to bolster food allergy awareness – one for a girl and one for a boy (they may take a few seconds to download).
- FARE Printable Food Allergy Awareness Posters – Their free downloadable posters for youth, teens, adults, and general fact awareness are now all in one place.
- Common Symptoms of Anaphylaxis – An at-a-glance poster with action item list by the Food Allergy & Anaphylaxis Connection Team (FAACT).
- Food Allergy Awareness Bookmarks – Also available from FAACT.
- More Food Allergy Posters – An assortment from Allergy Home (all free!).
- The Secret to Decoding Food Labels – A real world explanation of what food labels and allergen statements mean.
- Understanding “May Contain” Statements – This is ESSENTIAL reading for anyone who reviews ingredients for top food allergens or uses food allergen labels.
- Top 9-Free Meal Challenge – Invite friends and family to go top allergen-free for just one meal, or even a full day to experience just one aspect of the challenges that food allergy families face.
- Trigger Project – Awareness videos or children with food allergies.
Milk Allergies are Real!
Despite being one of the top eight allergens, and increasing in prevalence each year, milk is often ignored as an allergen. When you run across someone who doesn’t believe, help them gain some Respect for Milk Allergies and educate them on how Milk Allergy is a Leading Cause of Anaphylaxis AND Awareness.

24 Comments
The link to Apple Cider Vinaigrette Coleslaw doesn’t work, and I can’t find the recipe on that site.
Hi Vicki, Allergic Living removed it because it contains mustard, so I added it on our site! Link is good now. It’s here -> https://www.godairyfree.org/recipes/apple-cider-vinaigrette-coleslaw
Pingback: Gluten-Free Dairy-Free Crepes Recipe with a Vegan Option
Pingback: 5 great ways to create Food Allergy Awareness this week! | Allergy Free Zone
Pingback: Vegan Cinnamon Streusel Dessert Pizza Recipe - Go Dairy Free
Pingback: Easy DIY Candy Bars Recipe (Allergy-Friendly!) - Go Dairy Free
Pingback: Tropical Mango Sorbet Recipe (Dairy-Free)
This is an awesome resource! Sharing in Monday’s Link Love post!
Thank you so much Jessica!
Pingback: 6 Delicious Gluten Free and Dairy Free Bread Recipes
This is awesome, Alisa! From the infographic to the recipes – this is so valuable. Can’t wait to share it with my readers!
Thank you on all accounts Alyssa!
I developed an apparent allergy to chili peppers as an adult. I get an immediate anaphylactic type reaction. For more fun I just tested positive for Celiac. These recipes will be very helpful. I just wish I knew of a good substitute for the chili’s.
Oh no! That must be a frustrating wrench thrown into your eating patterns Karen! Believe it or not, I was recently caring for a relative who we discovered was severely allergic to chili peppers. They can definitely be hard to avoid when dining out, but at home it wasn’t too challenging. Though not identical, we found that paprika, smoked paprika and peppercorns were able to fill the void when absolutely needed. Glad the post is helpful for you!
Thank you very much for this very informative post and the accompanying delicious allergen-free recipes! Pinned.
Thanks for the pin and glad you like the post!
I love the references and the information in here. When my daughter was born she had an allergy to the protien in cow’s milk. Subsequently the pediatrician informed me that most likley any other children i have will have the same allergy. While i plan on nursing, that means I will need to give up all dairy products as well, so i love seeing fun and easy recipes i can make but that my whole family will enjoy.
Thanks!!
Hi Katie, so awesome that you are astute to the needs in advance! Yes, there are just TOO many amazing dairy-free recipes and meals!!
Really great information, Alisa! Thanks so much for sharing it 🙂
Thank you Susan!
Food Allergy awareness is so important. I love recipes that include everyone!
Me too 🙂
Pingback: Food Recipes | Food Recipes
Pingback: Food Allergy Awareness Week: Recipes and Resources - The Recipe Daily